Information for Medical professionals
Fontan procedure – Overview
The Fontan procedure or Total Cavopulmonary Connection is a palliative treatment option for children who are diagnosed with functionally univentricular congenital heart disease. The surgery includes various techniques, that ultimately result in a connection between the Vena cavae/ atrium to the Pulmonary circulation so that systemic venous blood bypasses the heart and goes directly to the lungs. The technique was originally described by Professor Francis Fontan in the year 1971 as palliation for children with Tricuspid atresia. What started as a surgery for extremely limited indications, has in recent years been used to help children with a wider range of anatomies. Patients need to be carefully selected to ensure optimal surgical outcomes.
Anatomy, Physiology and Indications for Surgery
In the spectrum of congenital heart disease, there are cardiac defects, that result in an anatomically or functionally single ventricle. This single ventricle performs the function of pumping blood to the lungs and the rest of the body. This causes the deoxygenated systemic venous return to mix with the oxygenated pulmonary venous blood within the heart, leading to a cyanotic state and the complications of a long-standing cyanotic state.
The concept of a Cavopulmonary connection is to make the systemic deoxygenated blood passively return to the lungs by directly connecting the veins to the pulmonary circulation, thereby bypassing the heart. This separates the deoxygenated blood from the oxygenated blood and also allows the functionally single ventricle to apply all energy to supplying systemic arterial flow which is now oxygenated. The Fontan circulation works only if the ventricle is functional, pulmonary resistance is low, and there is no obstruction along the pathway.
The common anatomical variations that result in the single ventricle physiology are Tricuspid atresia, Hypoplastic left heart syndrome, Double Inlet Ventricles, Pulmonary atresia, Unbalanced AV canals, etc. The spectrum of cardiac anomalies may be associated with other systemic anomalies, a condition known as Heterotaxy syndromes.
Indications:
Cardiac defects for which the Fontan completion procedure may be considered include:
- Tricuspid atresia
- Hypoplastic left heart syndrome (most common)
- Hypoplastic right heart syndrome
- Pulmonary atresia with intact ventricular septum
- Double-inlet left ventricle
- Double outlet right ventricle
- Unbalanced atrioventricular canal defects
- Ebstein anomalies that are adequate for Fontan correction
- Congenitally corrected transposition of the great arteries
Optimal physiologic and anatomical considerations such as the absence of valve anomalies, good ventricular function, normal pulmonary vascular resistance, and adequately sized pulmonary arteries are some of the technical factors that are decisive for suitability for surgery.
Contraindications:
In some of these conditions, the creation of a Fontan circulation can be challenging and cause increasing morbidity or mortality and therefore Fontan surgery has to be decided on a case-by-case basis.
- Pulmonary artery hypoplasia
- Left ventricular dysfunction and significant mitral regurgitation
- High pulmonary vascular resistance
Elevated pulmonary artery pressures can lead to less favorable surgical outcomes after Fontan.
Altered Physiology after a Fontan Completion surgery:
As mentioned before, the creation of a Fontan circulation separates the deoxygenated and oxygenated blood and retains the single functioning ventricle as the systemic ventricle. For proper function, this circulation relies on low pulmonary vascular resistance and preserved ventricular function. However, prolonged Fontan circulation can ultimately result in "failure" with reduced preload, increased systemic venous pressure, and chronic low cardiac output over a while.
To identify children who are ideal candidates for Fontan circulation and those who will benefit from this surgically and physiologically intense procedure, a staged approach helps. From the time of birth, these children may require multiple surgical procedures before culminating in the Fontan procedure. These usually include a Pulmonary artery banding, a BT shunt, a Glenn procedure (superior cavopulmonary connection), or a Norwood procedure as the case may be. Before the final surgery of Fontan completion, the pulmonary artery and ventricular pressures serve as guides for identifying candidates who will truly benefit.
Procedure Details:
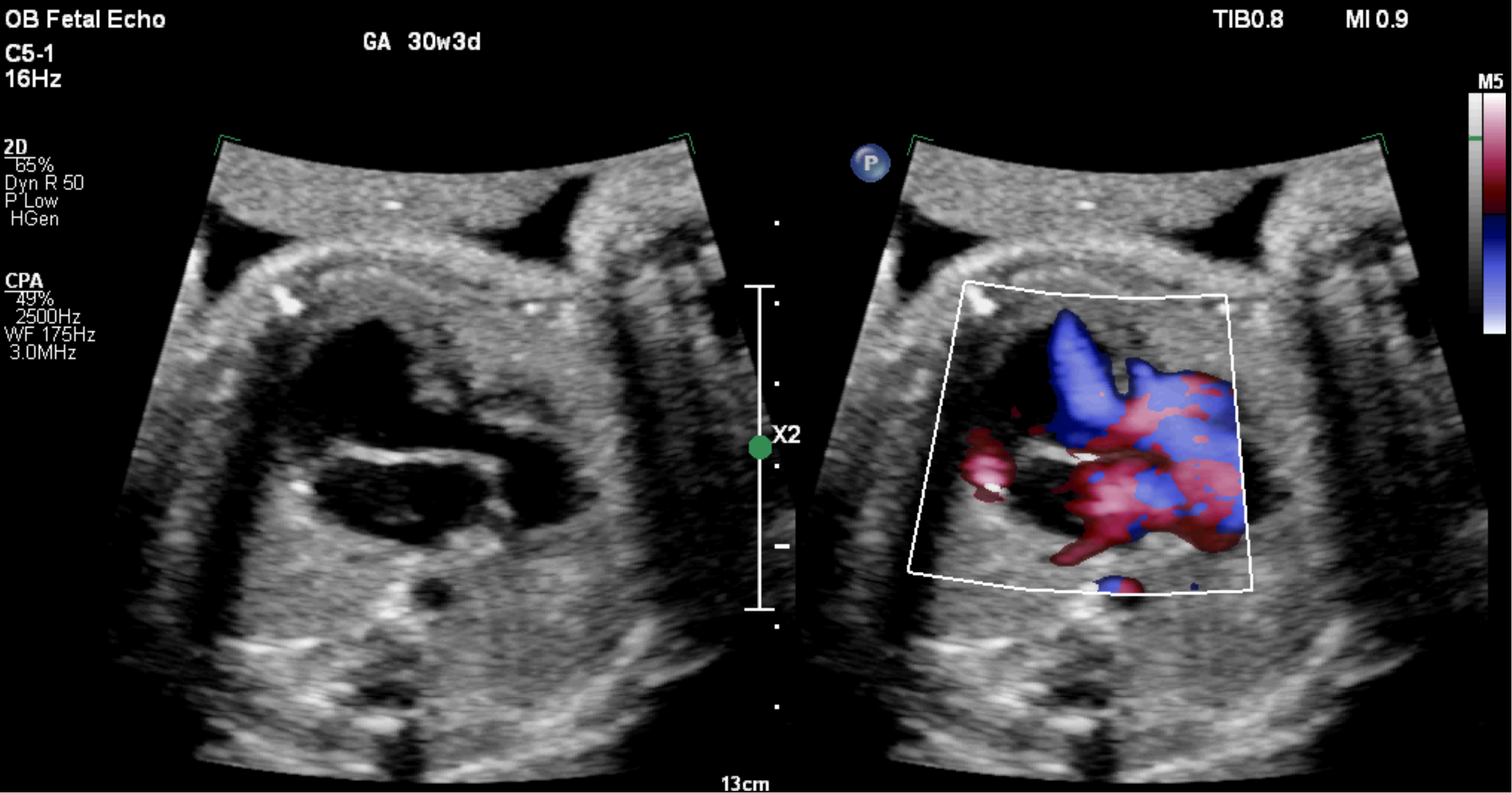
Pre-operative testing includes electrocardiography, transthoracic echocardiogram, CT scan, and cardiac catheterization. Most Fontan completion surgeries are considered high risk in view of the re-operative surgery and the abrupt change in physiology post operatively.
Surgery is performed under general anesthesia, endotracheal intubation, and appropriate invasive line monitoring (arterial line, central line, etc.) Patients are placed in a supine position, and a median sternotomy (usually re-operative) is performed.
Patients are cannulated in preparation for cardiopulmonary bypass.
Either of the modifications to create a Fontan circuit; an extracardiac conduit or a lateral tunnel technique or an Intra cardiac Extracardiac Fontan technique may be employed based on the anatomy of a given patient. The lateral tunnel is created intra-cardiac, within the atrium with a baffle to connect the inferior vena cava and the pulmonary artery. The extracardiac technique involves the placement of an appropriate-sized graft outside the heart to connect the inferior vena cava to the pulmonary artery. The use of the extracardiac technique appears to decrease the risk of atrial arrhythmias. Sometimes a "fenestration" is created, which is a connection from the extracardiac conduit to the right atrium, which acts as a pop-off between the two circulations and helps tide over the variations in pressures between the two systems.
Risks/ Benefits:
Fontan surgery has an estimated operative mortality of 1.2% and an average length of stay of 13 days for the Fontan procedure internationally. The mortality risk is highest in the first 5 years. Survival rates were 82% for the first year, 74% for the 5-year, and 71% for 10-year survival.
Immediate postoperative complications include the following:
- Hemorrhage
- Arrhythmias
- Pleural effusions
- Hepatic fibrosis
- Heart failure
- Chylothorax
- Cyanosis of the body
- Exercise intolerance
- Aortic root dysfunction
- Ventricular dysfunction
- Pulmonary vascular dysfunction
- Protein-losing enteropathy (PLE)
- Thromboembolism
- Kidney disease
- Liver disease
- Venous insufficiency
- Death
Recovery and Outlook:
The surgery is life-saving, although there are physiologic disturbances that affect the rest of the body and result in short-term and long-term complications. Multiple risk factors have been identified that may contribute to increased mortality, takedown, or transplantation rates. Identifying the ideal candidates and modifying and treating the risk factors can reduce the morbidity and mortality.
